Dental Implants have shown to achieve high success rates long-term but like all treatment modalities, they are also prone to complications. These could arise from improper planning, lack of understanding of correct surgical and prosthetic implementation, improper post-implantation care as well as material failures. Clinically most implant problems present as biologic complications broadly categorized into Peri-implant mucositis and Peri-implantitis. There are circumstances where mechanical complications such as loosening of the crown or fractures of screws may not produce biologic signs of disease.
Peri-Implant Health
Peri-implant health has been measured with similar parameters used to define periodontal health around teeth. However, in-depth understanding of the differences in peri-implant tissues compared to those of natural teeth is vital to prevent overdiagnosis of disease conditions and subsequent therapy recommendations. Peri-implant health is characterized by an absence of clinical presence of inflammation and bleeding on probing and this can exist around implants regardless of bone levels. As probing depths of the sulcus around implants is influenced by many factors other than disease processes (such as abutment height or height of soft tissue) a range of probing depths for peri-implant health is difficult to define.
Peri-Implant Mucositis
Peri-implant mucositis is characterized by bleeding on probing and visual signs of inflammation. While there is strong evidence that peri-implant mucositis is caused by plaque, there is also some limited evidence for non-plaque induced peri-implant mucositis. Typically when probing around the implant there will be spontaneous bleeding and the mucosa may be tender. Peri-implant mucositis is a reversible condition much like gingivitis in natural teeth with simple measures that aim at eliminating plaque.
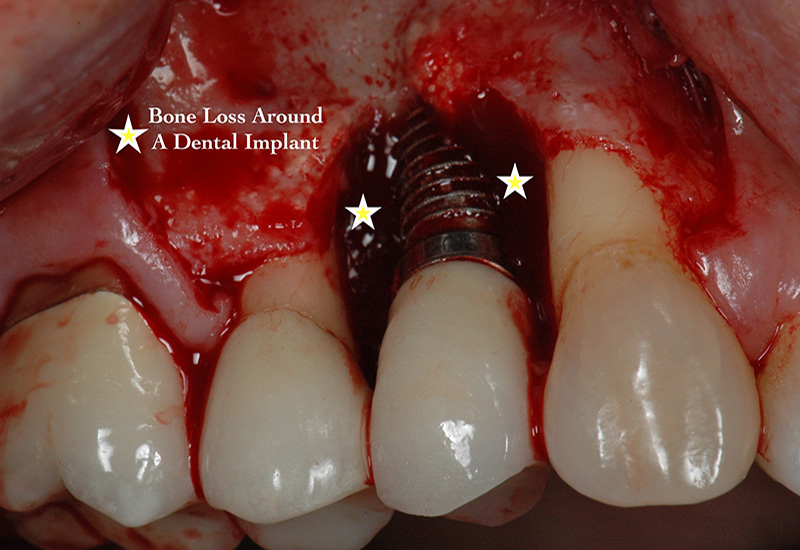
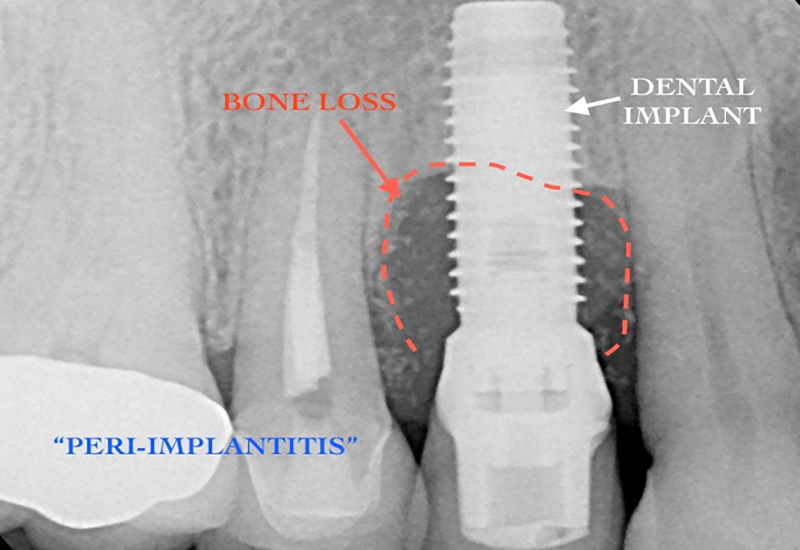
Peri-Implantitis
Peri-implantitis is a destructive condition occurring in soft and hard tissues around dental implants, similar to periodontal disease seen around teeth, which may ultimately lead to implant failure if not treated. It is characterized by inflammation and bleeding in the peri-implant tissue and progressive loss of supporting bone observed radiographically. It is believed that it is preceded by peri-mucositis. It has been reported that peri-implantitis occurs on the order of 10% of implants and in 20% patients within 5 years to 10 years after implant placement. The onset may occur early or late in the healing phase or at any point after the implant has been in function. A close follow-up post-treatment is, therefore, necessary to ensure optimal healing and to address any early signs of disease.
Peri-implantitis may progress in a non-linear fashion and clinically manifests with bleeding and an increase in probing depths compared to baseline measurements taken 1yr after the restorative phase is completed. There is strong evidence that there is an increased risk of developing peri-implantitis in patients who have a history of chronic periodontitis, poor plaque control skills, and no regular maintenance care after implant therapy. Although analysis of recent data remains inconclusive, factors such as smoking and uncontrolled diabetes may put patients undergoing implant treatment at higher risk for peri-implantitis. Other factors that may increase the incidence of developing peri-implantitis include the presence of cement under the gum margins after placement of crowns and absence of a thick band of dense tissue around the neck of the implant that provides protection to the underlying bone and makes oral hygiene practices easier.
Therapy
Peri-implant mucositis and peri-implantitis differ with respect to treatment. Evidence suggests that peri-implant mucositis can be successfully treated if detected early and when combined with effective non- surgical efforts. Non-surgical therapy has not been shown to be effective for the treatment of peri-implantitis. Therefore, various surgical treatment modalities have been proposed and have shown promising results. These invariably involve reflecting the gum back to gain access to the implant body and begin decontamination of the infected implant surface. Subsequent treatment would include evaluation of occlusion and, if necessary, recontouring and regeneration of the bone to stabilize the supporting hard and soft tissues of the implant. In most cases, a bone graft is necessary to replace the lost bone. In very advanced stages of Peri-implant bone loss, it may not be feasible to successfully treat the ailing implant and the implant must be removed. The site of implant removal will be bone grafted and after a suitable healing phase, a new implant can be placed if that is desired.
LAPIP™ (Laser Assisted Peri-Implantitis Procedure)
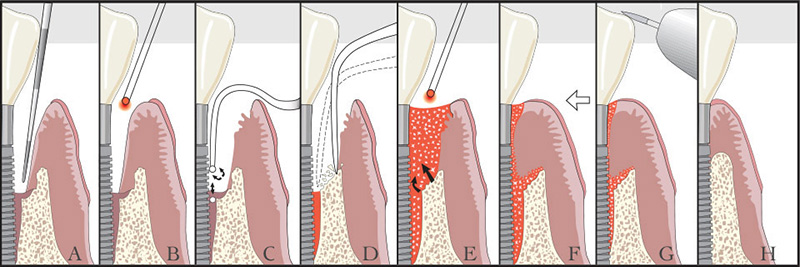
A. Perio probe indicates excessive pocket depth.
B. Laser vaporizes bacteria, diseased tissue, pathologic proteins, and titanium corrosion contaminants in soft tissue.
C. Ultrasonic scaler tips are used to remove surface accretions.
D. Bone is modified at time of surgery.
E. Laser is used to form a stable fibrin blood clot containing stem cells from bone.
F. Adhesion to clean surface, with a stable fibrin clot at the gingival crest to create a ‘closed system’.
G. Occlusal trauma is adjusted.
H. New attachment is regenerated.
A novel minimally invasive technique, In specific cases it may be possible to achieve favorable outcomes and overcome the many challenges of peri-implant disease therapy with the use of Lasers. LAPIP® (Laser Assisted Peri-Implantitis Procedure) is a modification of the LANAP® (Laser Assisted New Attachment Procedure) protocol. The PerioLase® MVP-7TM is able to target and remove the dark pigmented, diseased tissue around the affected dental implant.
If you have been told that you have Peri-Implantitis, Call our office today to schedule an appointment and see if LAPIP™ may be a suitable solution for you.
