Periodontal Health
Periodontal Health
Periodontal health should be defined as a state free from inflammatory periodontal disease (physical or mental). This, in turn, means that absence of inflammation associated with gingivitis or periodontitis, as determined clinically, is a prerequisite for defining periodontal health.
Defining periodontal health is very important if we are to have a common reference point for assessing periodontal disease and determining meaningful treatment outcomes. Health can be evaluated at both the histological and clinical levels and should be considered in the context of a preventive starting point and a therapeutic endpoint.
No longer can periodontal diseases be considered simple bacterial infections. Rather, they are complex diseases of multifactorial nature involving an intricate interplay between the subgingival microbiota, the host immune and inflammatory responses, and environmental modifying factors. Thus, periodontal health must not be considered solely in the context of plaque/bacteria levels and control but must embrace a holistic consideration and evaluation of all factors responsible for the emergence of the disease, as well as the restoration and maintenance of health.
Determinants of periodontal health fall into three (3) primary categories:
- Microbiological
- Host
- Environmental
For the purpose of this guide on Periodontal Disease, we will only consider the clinical indicators of clinical periodontal health.
The relevance of recognizing such important determinants of periodontal health and disease as controllable and uncontrollable predisposing and modifying factors cannot be under-estimated, and their assessment for each patient is crucial to attaining and maintaining clinical periodontal health.
In this context, predisposing factors are defined as any agent or condition that contributes to the accumulation of dental plaque (eg, tooth position, dental restorations, tooth anatomy). Modifying factors are defined as any agent or condition that alters the way in which an individual responds to subgingival plaque accumulation (eg. smoking, medications, systemic conditions). The thresholds to establish when such factors are controlled versus not fully controlled await further elaboration, but it is reasonable to expect that many factors will be determined controllable (eg, good control of diabetes, smoking cessation, removal of overhangs) while others will not (eg, immune system, genetic predisposition, and use of vital medications).
Microbiological Determinants of Clinical Periodontal Health
Supragingival plaque composition
Subgingival biofilm composition
Host Determinants of Clinical Periodontal Health
Local predisposing factors
- Periodontal pockets
- Dental restorations
- Root anatomy
- Tooth position and crowding
Local predisposing factors
Systemic modifying factors
- Host immune function
- Systemic health
- Genetics
Environmental Determinants of Clinical Periodontal Health
Smoking
Medications
Stress
Nutrition
The 4 Levels of Periodontal Health
There are four (4) levels of periodontal health, depending on the state of the periodontium (structurally and clinically sound or reduced) and the relative treatment outcomes.
Pristine periodontal health, with a structurally sound and uninflamed periodontium
Well-maintained clinical periodontal health, with a structurally and clinically sound (intact) periodontium
Periodontal disease stability, with a reduced periodontium
Periodontal disease remission/control, with a reduced periodontium
Forms of Periodontitis
Necrotizing Periodontal Diseases
- Necrotizing Gingivitis
- Necrotizing Periodontitis
- Necrotizing Stomatitis
Periodontitis as Manifestation of Systemic Diseases
The classification of these conditions should be based on the primary systemic disease according to the International Statistical Classification of Diseases and Related Health Problems (ICD) codes.
Periodontitis
- Stages: Based on Severity and Complexity of Management
Refer to Chapter 2 in this guide for further descriptions of the following four stages.
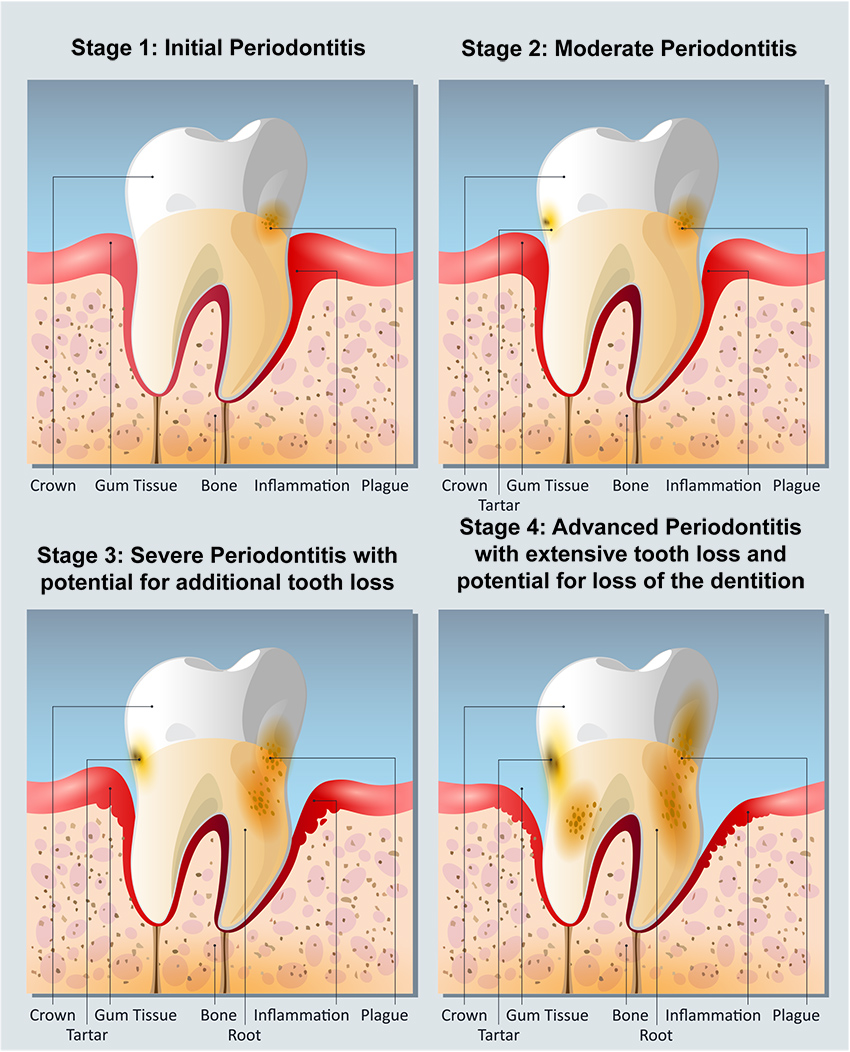
- Stage 1: Initial Periodontitis
- Stage 2: Moderate Periodontitis
- Stage 3: Severe Periodontitis with potential for additional tooth loss
- Stage 4: Severe Periodontitis with potential for loss of the dentition
- Extent and distribution: localized; generalized; molar-incisor distribution
- Grades: Evidence or risk of rapid progression, anticipated treatment response.
- Grade A: Slow rate of progression
- Grade B: Moderate rate of progression
- Grade C: Rapid rate of progression
- Stages: Based on Severity and Complexity of Management
Oral Hygiene
Good oral hygiene has always been considered a mainstay of periodontal health. It is usually achieved by a combination of good personal oral hygiene and regular professional care. It must be remembered that plaque accounts for only 20 percent of the direct risk of developing periodontitis, thus it must not be forgotten that the remaining 80 percent of the direct and indirect risk and modifying factors may be responsible for the development of periodontal diseases. While oral hygiene remains the most important factor in obtaining and maintaining periodontal health, it should not be the sole focus of attention.
Additional factors must be addressed in the quest for attaining or maintaining periodontal health.
Source: Journal of Periodontology, Lang and Bartold, page 812
Types of Gum Disease
What is Gum Disease?
Gum disease is the infection and inflammation of gums and underlying support structures in the periodontium, such as the alveolar jaw bone, as a result of bacteria, fungi, or other pathogens.
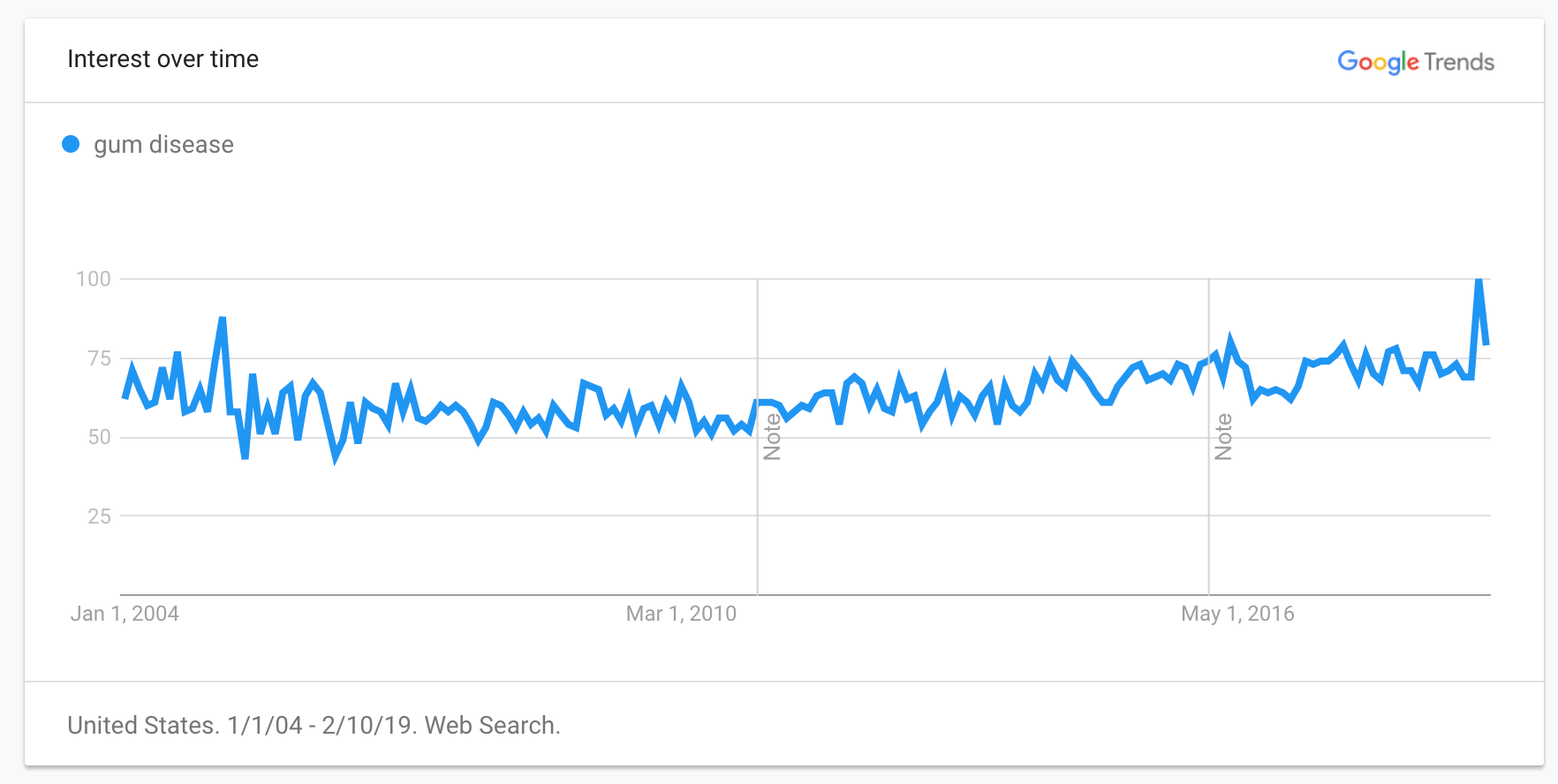
Gum disease according to Google Trends is near its peak popularity in regards to search terms on the Internet.
Pathology of Gum Disease
While there are many potential pathogens responsible for individual cases of gum disease, by and large, the vast majority of gum disease cases, from early-stage gingivitis to moderate-severe stage periodontitis, are the result of bacterial action.
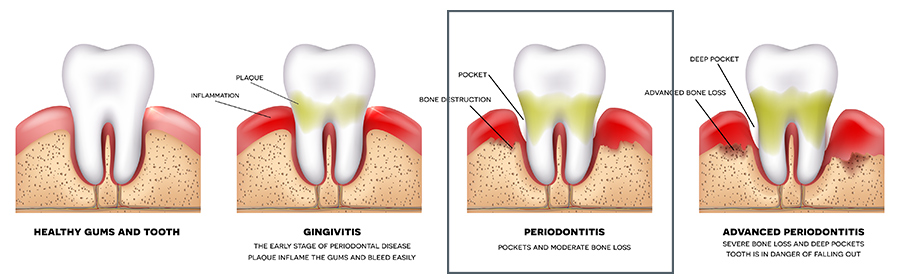
Typically this occurs in distinct stages with corresponding characteristics.
Healthy Gums
- Gums will be coral pink in color
- Gums will hug the teeth tightly
- Gums will not bleed on probing
- Gum pockets all measure to a normal 3mm or less
Gingivitis
In the initial stage of gum disease, also known as gingivitis, the buildup of plaque and a microbial biofilm along the gum line leads to inflammation, swelling, redness, and mild sensitivity.
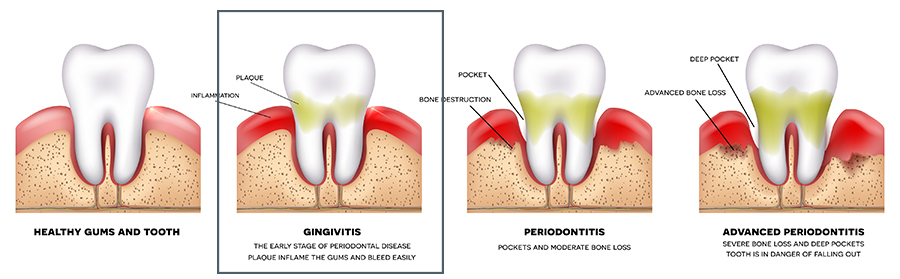
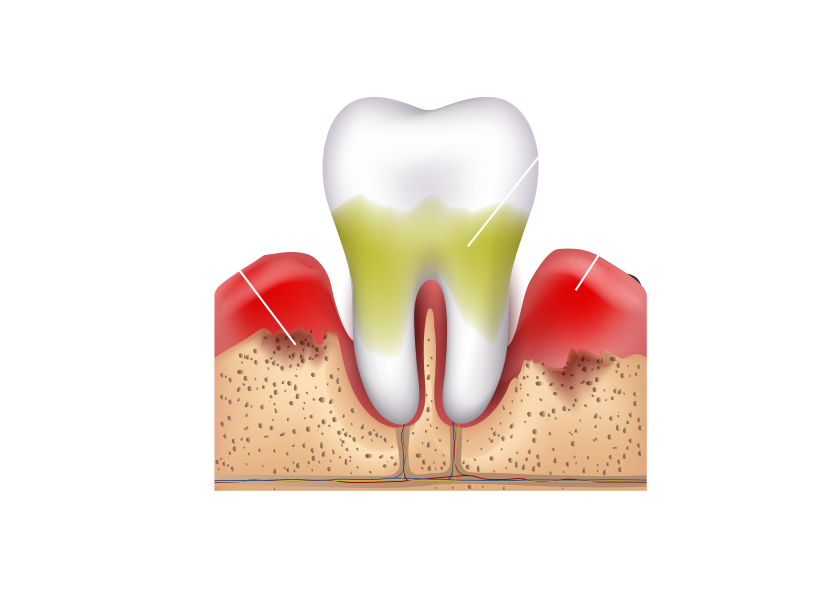
Periodontitis
Once bacteria penetrates beneath the gum line, gum disease can become periodontitis or an infection deep within the soft tissues that can attack the underlying periodontal bones.
The typical progression from gingivitis to periodontitis is characterized by the gradual recession of the gums, making dental roots more vulnerable to infection and the development of gum pockets, which can develop into abscesses.
The health implications of gum disease are many and varied and affect not only the teeth and mouth but the body as a whole.
Signs of Periodontal Disease
- Gums that bleed when you brush or floss your teeth
- Red, swollen or tender gums
- Pus between your teeth
- Pain when chewing
- Calculus or tartar build-up
- Changes in bite
- Loose or shifting teeth
- Bad breath or chronic bad taste
- Teeth sensitivity to hot or cold
- Gums that recede or gums that shrink away from your teeth
Moderate to Advanced Periodontitis
Within the mouth, untreated gum disease will eventually progress into severe, advanced-stage periodontitis. Bone destruction and complete edentulism are common at this late stage of the disease. The disfiguration and damage of the gums and soft tissues can have destructive health effects on the entire mouth, compromise a person’s ability to eat, chew, and speak, and also have many severe psychological effects on self-confidence and self-esteem.
Gum disease also has far-reaching health consequences outside the mouth itself. Periodontal infections can directly spread into the bloodstream via the periodontium resulting in sepsis and potentially fatal septic shock.
Gum disease is also implicated as either a co-factor, exacerbating condition, or direct cause of a variety of systemic human disorders from diabetes to heart disease.
Gum Disease Conditions
Bacteria associated with periodontal gum disease, for example, have been found on the heart valves of those diagnosed with gum disease, and are responsible for endocarditis.
Other conditions associated with gum disease:
Bad breath
Gum recession
Tooth loss
Facial deformation
Bone loss
Stroke
Premature birth
While gum disease is often associated with the mouth and teeth, the condition has far-reaching effects and severe consequences. However, it is mostly a preventable disease. With a rigorous oral hygiene routine and appropriate professional attention from a certified periodontist or periodontal specialist, periodontal gum disease can be cured or even reversed in some cases. Cosmetic damage from moderate to severe cases of gum disease can often be remedied with cosmetic dentistry procedures such as periodontal implants to replace lost teeth.
Don't Ignore Your Oral Health
If you value your oral as well as your overall health, a periodontal evaluation is a good idea. Sometimes the only way to detect periodontal disease is through a periodontal evaluation. A periodontal evaluation may be especially important to you for the following reasons:
- Notice any symptoms of periodontal disease.
- Have heart disease, diabetes, respiratory disease or osteoporosis.
- Are thinking of becoming pregnant.
- Have a family member with periodontal disease. Research suggests that the bacteria that cause periodontal disease can pass through saliva. This means the common contact of saliva in families puts children and couples at risk for contracting the periodontal disease of another family member.
- Have a sore or irritation in your mouth that does not get better within two (2) weeks.
Gum disease is an umbrella term that is often used to describe an infection of the gums, soft tissues, and sometimes, the periodontal bone itself. However, the precise severity, location, and general conditions of pathology will differ from one case to another. As a result, treatments and therapies must often be tailored to match each patient's individualized oral conditions.
To make sense of the general diagnosis of gum disease, it is helpful to categorize the disease into four classifications of periodontitis:
Stage 1: Initial Periodontitis
Initial periodontitis is defined as gingival inflammation without periodontal attachment loss. Clinical signs include redness, swelling, and bleeding on gentle probing. Stage 1 periodontitis is the borderland between gingivitis and periodontitis and represents the early stages of attachment loss. As such, patients with Stage 1 periodontitis have developed periodontitis in response to the persistence of gingival inflammation and biofilm dysbiosis.
Early diagnosis offers opportunities for early intervention and monitoring. Early diagnosis may be a formidable challenge in a general dental practice setting where the current gold standard for defining periodontitis may be inaccurate. Assessment of salivary biomarkers and new imaging technologies often increase early detection of Stage 1 periodontitis in a variety of settings.
Characteristics of Gingivitis
- Mild inflammation of the gums caused by plaque build-up
- Gums may be red and/or sore
- Gums will bleed while brushing or during probing
- Inflamed sensitive gums
- Possible bad breath/taste
- No damage to the supporting bone in this stage
Initial Periodontitis
- If left untreated, the gum infection damages the bone and supporting tissues
- Gum separates from the tooth and the bone level deteriorates
Stage 2: Moderate Periodontitis
Stage 2 represents established periodontitis in which a carefully performed clinical periodontal examination identifies the characteristic damages that periodontitis has caused to tooth support.
At this stage of the disease process, however, management of periodontitis remains relatively straightforward for many cases as the application of standard treatment principles involving regular personal and professional bacterial removal and monitoring is expected to arrest disease progression. Careful evaluation of the patient's response to treatment is essential to help guide and assess more intensive management based on treatment outcomes.
Characteristics of Moderate-Severe Periodontitis
- Gums recede farther and separate
- Pus may develop, bone loss continues, and teeth may loosen or fall out
- Teeth may become mobile or loose
- Constant bad breath and bad taste
- Pockets larger than 6mm deep
- Some teeth may need to be extracted
- Severe bone loss and tooth support
Stage 3: Severe Periodontitis with potential for additional tooth loss
At Stage 3, periodontitis has produced significant damage to the attachment apparatus and, in the absence of advanced treatment, tooth loss may occur.
This stage is characterized by the presence of deep intrabony defects, furcation involvement, history of periodontal tooth loss/exfoliation, and the presence of localized ridge defects that complicate implant tooth replacement.
In spite of the possibility of tooth loss, the masticatory function is preserved, and the treatment of periodontitis does not require complex rehabilitation of function.
Stage 4: Advanced Periodontitis with extensive tooth loss and potential for loss of the dentition
At the more advanced Stage 4, periodontitis causes considerable damage to the periodontal support and may cause significant tooth loss.
In the absence of proper control of the periodontitis and adequate rehabilitation, the dentition is at risk of being lost.
This stage is characterized by the presence of deep periodontal lesions that extend to the apical portion of the root and history of multiple tooth loss; it is frequently complicated by tooth hypermobility due to secondary occlusal trauma and the sequelae of tooth loss. Often, management requires stabilization/restoration of masticatory function.
This helps describe the progressive nature of the disease.
Gum disease can also be categorized into 5 different types depending on specific characteristics of the disease. One patient’s periodontal disease, for example, may be highly invasive and spread rapidly throughout the jaw. Another patient’s gum disease may manifest as a series of highly localized and contained abscesses. The goal in this chapter is to help you make sense of gum disease in its varying forms.
4 Stages of Gum Disease (Periodontal Disease)
One of the most effective ways to categorize periodontal disease is to do so chronologically. Each chronological “stage” of the disease can be easily and readily defined with specific characteristics including signs and symptoms. However, it is important to note that the three stages we describe do not have distinct borders. Patients can, for example, experience symptoms of early-stage gum disease (gingivitis) while also displaying signs of moderate gum disease. These descriptions are general in nature and not intended for patients to self-diagnose.
When in doubt, the best way to confirm a suspicion of gum disease is to visit your local dental clinic for a professional checkup. A dentist or periodontist will be able to tell you instantly whether or not you have gum disease and how advanced it is, as well as treatments and procedures to combat it.
Early-stage gum disease, also commonly referred to as gingivitis, is characterized by visible redness, swelling, and bleeding in the gums as well as minor discomfort in some situations. Sure signs of gingivitis include bleeding when brushing or sensitivity when flossing.
Chronologically, gingivitis constitutes the earliest form of gum disease and is the easiest and most effective stage of the disease to treat. Damage incurred can be reversed with no permanent scarring or signs of damage. However, if left untreated, early-stage gum disease can progress over time into middle and late-stage gum disease which becomes more difficult to treat or reverse the damage.
Stage 3 gum disease occurs when gingivitis progresses into full-blown gum disease. By this stage, damage to the gums is both visible and permanent. Delamination of the gums from the underlying periodontal bone is apparent and often characterized by gum recession or the formation of gum pockets beneath the gum line.
Gum pockets are small areas of interstitial space formed when the gum tissues have detached, as a direct result of bacterial action, from the dental bone. The presence of gum pockets is particularly troublesome as they are difficult to clean and readily trap both bacteria and food debris. Over time, the gum pockets can become infected and lead to advanced-stage periodontitis.
Advanced-stage or late-stage gum disease, also known as periodontitis, occurs when oral infections have migrated deep into the soft tissues and are actively attacking the periodontal bone beneath.
Advanced periodontal disease is characterized by bone loss, tooth loss, necrotic tissues, and severe gum recession.
Symptoms include extreme dental pain, loose teeth, facial swelling, bleeding, fever, blood infections, abscesses, and the drainage of pus into the oral cavity.
Advanced-stage periodontal disease often results in complete edentulism or total tooth loss.
Gum Disease: Symptoms & Causes
Gum disease is an infection of the tissues that hold your teeth in place. It is common but largely preventable. It is generally the result of poor oral hygiene, such as poor brushing and flossing habits that permit plaque -- a sticky film of bacteria --- to build up on the teeth and harden.
In advanced stages of gum disease, periodontal disease can lead to sore, bleeding gums; pain when chewing, and even severe tooth loss.
Symptoms of Gum Disease
Gum disease can progress into periodontitis, to avoid this progression it is important to recognize the signs of gum disease. Following are the most common signs of gum disease.
Red, swollen or tender gums or other pain in your mouth
Bleeding while brushing treeth, flossing, or eating hard food
Persistent sores in your mouth
Bad breath
Loose or separating teeth
Pus between your gums and teeth
A gradual change in the way your teeth fit together when you bite
Sensitivity when brushing or flossing along the gumline
The visible buildup of plaque along the gumline
Gum pockets (pocket of space between gums and teeth)
Gum recession
Causes of Gum Disease
Gum disease is largely the result of a buildup of bacteria on the gums and especially along the gum line where the gums meet the tooth.
Bacteria, usually in the form of plaque or tartar, forms a thin biofilm on the gums and teeth as they feed off of food debris. As plaque grows, it produces toxic waste products that irritate the soft tissues of the gums. Plaque can harden into tartar beneath your gum line. This causes your body’s tissues to react with the symptoms mentioned above. These symptoms are your body’s way of warning you that something is wrong in your mouth.
Eventually, these bacterial toxins will cause your gums to recess. Bacteria most implicated in this process are mostly anaerobic bacteria, particularly Fusobacteria and spirochete species. These are notably different species than those responsible for dental cavities. This points to the importance of controlling bacteria in every part of the mouth through a rigorous dental hygiene routine and regular visits to a dental professional.
While bacteria is the root cause of gum disease, there are other factors you should be aware of which include the following:
Plaque
Gum disease is most commonly caused by plaque which is a thick film of bacteria forming on gums and teeth. Brushing, flossing, and rinsing on a regular basis as well as seeing your dentist for regular checkups and cleaning will mitigate plaque growth.
Medications
Prescription medications may have a side effect of hindering normal production of saliva, creating a dry mouth where bacteria often thrive and spread. If you fall into this category I recommend you see your dentist or periodontist.
Diet
A diet that is high in sugar and carbohydrates and low in water and vitamin C is a sure sign of greater chances of developing gum problems.
Loose or Crooked Teeth
Misalignment or pockets between teeth create more opportunities for plaque to thrive and eventually further damage teeth and gums. Good oral hygiene is a must but often brushing and flossing is not enough to reach the pockets around the teeth. I recommend regular visits to your dentist and a good Waterpik or water flosser.
Family History of Gum Disease
If you have a family history of gum disease, this is important to mention to your periodontist and dentist. A family history of gum disease may put you at a slightly increased risk of developing a bacterial infection.
Tobacco Use
Smoking, vaping, or chewing tobacco prevents the gum tissue from being able to heal.
Stress
Stress impairs the body's immune response to bacterial growth.
Mouth Breathing
Regular breathing from your mouth can be harsh on the gums when they aren't protected by the lips, causing chronic inflammation and irritation.
Cancer
Cancer and cancer treatment can make a person more susceptible to infection and increase the risk of gum disease. If there is a past history of cancer personally or in your family be sure to inform your dentist or periodontist.
Pregnancy
Hormonal changes in puberty, pregnancy, and menopause typically correlate with a rise in gum disease or gingivitis. The increase in hormones causes the blood vessels in the gums to be more susceptible to bacterial and chemical attack. At puberty, prevalence of gum disease ranges between 70 to 90 percent.
Diabetes
Diagetes mellitus hinders blood circulation which affects the ability of the gums to heal.
Alcohol
Alcohol affects oral defense mechanisms which can result in poor circulation and the ability of the gums to heal.
Periodontitis: Symptoms and Causes
As we mentioned above, there are a few different types of periodontitis: chronic, aggressive, necrotizing, and periodontitis as a manifestation of systemic diseases.
These terms are relatively new and arose from the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. Renaming and reclassifying periodontitis helps periodontists, as well as patients, clearly distinguish between the more common types of periodontitis, which are chronic and aggressive, from the more uncommon types—necrotizing and when the disease is a manifestation of another systemic disease.
Generally speaking, periodontitis is caused by plaque build-up on the teeth. But other factors such as disease and family history can contribute to periodontitis. Let’s break down the symptoms and causes of each type:
Chronic Periodontitis
This is the most common type of periodontitis and is caused by plaque build-up.
Signs of chronic periodontitis include:
- Swollen gums
- Discolored gums—bright red or purple
- Bleeding gums
- Loose teeth
- New spaces between the teeth
- Difficulty chewing due to pain
- Pus between the teeth and gums
Aggressive Periodontitis
This type of periodontitis typically begins in childhood or young adulthood. It is as its name suggests—an aggressive form of periodontitis causing rapid bone loss. The cause of aggressive periodontitis is the presence of highly dangerous bacteria in the mouth. This type of periodontitis is hereditary in many cases.
Symptoms of aggressive periodontitis include:
- Severe tissue or bone loss
- Abnormal gaps in the teeth
- Pus between the teeth and gums
- Tooth sensitivity
- Toothache
- Bleeding gums
- Bad breath
- An abnormal taste in the mouth
Necrotizing Periodontitis
This type of periodontitis is also caused by plaque and bacteria but is linked to a suppressed immune system, often due to another serious health issue such as HIV, cancer, or malnutrition.
Symptoms of necrotizing periodontitis include:
- Severe pain in the mouth
- Spontaneous bleeding
- Bad breath
- Bone loss
- Low-grade fever
- Swollen lymph nodes
Periodontitis as a manifestation of systemic diseases
This type of periodontitis is often found at a young age and is associated with another disease such as heart disease, respiratory disease or diabetes. In some cases, the presence of periodontitis may point the patient’s doctor to the larger systemic disease at hand.
Symptoms of periodontitis as a manifestation of systemic diseases include:
- Loss of tissue
- Bone loss
- Inflamed gums
Health Risks of Gum Disease
Gum disease is one of the main causes of tooth loss and is highly prevalent; people are often unaware they have it because it is not painful and doesn't affect their daily life. But if left untreated the impact can be serious. It has also been linked to cardiovascular disease and type 2 diabetes as bacteria can enter the bloodstream through the mouth and spread inflammation through the body.
It is well established that there is a strong connection between periodontal disease and other chronic conditions such as osteoporosis, diabetes, heart disease, and stroke as well as respiratory issues. Periodontal disease is an inflammatory condition caused by bacteria within pockets around teeth that can cause one and soft tissue loss. Periodontal bacteria can enter the bloodstream and travel to major organs and begin new infections and chronic systemic health issues.
Research is suggesting that this may:
- Contribute to the development of heart disease, the nation's leading cause of death.
- Increase the risk of stroke.
- Increase a woman's risk of having a preterm, low birth weight baby.
- Pose a serious threat to people whose health is compromised by diabetes, respiratory diseases, or osteoporosis.

