Non-Surgical Therapy
Scaling and Root Planing
Some cases of acute periodontal (gum) disease that do not respond to more conventional treatment and self-care such as flossing may require a special kind of cleaning called scaling and root planing.
The procedure begins with administration of a local anesthetic to reduce any discomfort. Then, a small instrument called a "scaler," or an ultrasonic cleaner, is used to clean beneath your gum line to remove plaque and tartar.
The root surfaces on the tooth are then planed and smoothed. This lets the gum tissue heal and reattach itself to the tooth.
Studies have shown that non-surgical scaling and root planing is usually successful if the periodontal pockets are shallower than 4-5mm. It is necessary for the dentist or hygienist to perform a re-evaluation four to six weeks after the initial scaling and root planning to determine if the patient’s oral hygiene has improved and inflammation has regressed.
Pocket depths greater than 5-6mm which remain after initial therapy, with bleeding upon probing, indicate continued active disease and will likely lead to further bone loss. This is especially true in molar tooth sites where areas between the roots have been exposed. If non-surgical therapy is unsuccessful, periodontal surgery may be needed to stop progressive bone loss and regenerate lost bone where possible.
Antibiotics in the Management of Periodontal Disease
With some more advanced types of periodontal disease, we may recommend a week's course of antibiotics at the end of any deep cleaning, in order to eliminate more bacteria in the mouth so as to maximize the healing and pocket shrinkage.
Teeth Splinting
When the teeth are compromised from a periodontal point of view and have lost most of their bone and gum support due to periodontal disease, they become wobbly. As a result, the chewing efficiency, phonetics, and function are compromised. To increase patient comfort during chewing we can connect multiple teeth together (teeth splinting) to reduce mobility and improve the patient's function and chewing efficacy. To connect teeth to each other, the enamel surface of the tooth is etched and composite resin can then be bonded to the etched surface to rigidly connect the teeth to each other. The connection can be strengthened by adding a fiber or metal framework. No healthy tooth substance is removed.
Surgical Therapy
If non-surgical periodontal therapy is unsuccessful, periodontal surgery may be needed to stop progressive bone loss and regenerate lost bone where possible.
There are many surgical approaches used in the treatment of advanced periodontitis. Long-term studies have shown that in moderate to advanced periodontitis, surgically treated cases often have less further breakdown over time and when coupled with a Frequency of eating is also a factor because regular snacks and drinks can strip the teeth of their protective minerals, accelerating decay.
Even with a good tooth brushing technique, most people miss parts of their mouth regularly so it is recommended a dental check-up twice a year to detect and treat early signs of gum disease and hygienist appointments every quarter to remove calculus.
If you are experiencing bleeding gums, gums that have come away from the teeth, persistent bad breath or teeth that are loose or changing position, book your consultation.
Pocket Reduction Surgery
Your bone and gum tissue should fit snugly around your teeth like a turtleneck. When you have periodontal disease, this supporting tissue and bone are destroyed, forming “pockets” around the teeth. Over time, these pockets become deeper, providing a larger space for bacteria to thrive and wreak havoc.
As bacteria accumulate and advance under the gum tissue in these deep pockets, additional bone and tissue loss follow. Eventually, if too much bone is lost, the teeth will need to be extracted.
Flap surgery is sometimes performed to remove tartar deposits in deep pockets or to reduce the periodontal pocket and make it easier for you or your dental professional to keep the area clean. This common surgery involves lifting back the gums and removing the tartar. The gums are then sutured back in place so that the tissue fits snugly around the tooth again.
A pocket reduction prodecure is recommended if daily at-home oral hygiene and a professional care routine cannot effectively reach these deep pockets.
In some cases, irregular surfaces of the damaged bone are smoothed to limit areas where disease-causing bacteria can hide. This allows the gum tissue to better reattach to healthy bone.
In other cases, bone may be smoothed and reshaped so that plaque has fewer places to grow; and repaired (grafted) with bone from another part of the body or with man-made materials. A lining on the bone graft may be placed to help the bone grow back. The lining may need to be removed later.
The flap procedure should cure your gum disease if you maintain good dental care after the surgery. Your gums should become pink and healthy again.
Osseous Surgery
Osseous (meaning "bone") surgery involves removing and/or reshaping the jawbone under the gum. In some advanced cases, non-surgical debridement may not be sufficient. Further treatment in the form of periodontal surgery would be needed if there is severe inflammation and deep pockets. Surgical techniques are more advanced and generally minimally invasive.
The aim of periodontal surgery is to restore and regenerate the lost structures that support the tooth, these include, the soft tissue and bone. Gingival flap surgery is a type of gum procedure and is carried out if gum pockets do not respond to non-surgical therapy. Under such circumstances, pocket elimination is one of the most common surgical procedures used to treat periodontal disease.
To gain access to the deep periodontal pockets the gum is pulled back gently. The periodontist can then visualize and remove thoroughly all plaque and calculus (tartar). The bone cavities caused by the disease are smoothed over and the gum tissues are positioned even with the bone level to reduce the periodontal pockets and minimize the spaces under the gums where disease-causing bacteria can hide. Tiny sutures are placed to stabilize the new gum position.
A protective dressing often is placed around the teeth to cover and secure the surgical area. Sedation can be used to keep you comfortable and relaxed if needed. You will have a follow-up appointment in 7-14 days to remove any remaining sutures, evaluate your healing, and review oral hygiene. Three months after surgery you will have a periodontal cleaning.
Laser Periodontal Therapy
Dental lasers are a tremendous asset in soft tissue surgeries, including gingivectomy/gingivoplasty, frenectomy, soft tissue biopsies, gingival sculpting associated with periodontal plastic surgical procedures because of their proven hemostatic effect. Additionally, they have been used successfully in treatment of drug-induced gingival overgrowth either alone or in conjunction with conventional surgery.
Esthetic Smile Enhancement
Excessive gums, more commonly termed the “gummy smile”, can be simply, quickly and comfortably corrected using LASER gum treatment. Healing is usually complete in three days, and no adjustment to activity level or diet is necessary. The sensitive nature of the Waterlase MD Turbo YSGG laser can help minimize tissue displacement and flap preparation in osseous crown lengthening during a laser treatment for gum disease. It aids in carrying out an externally beveled gingivectomy, moulding the free gingival margin, troughing, and recontouring and smoothing the bone.
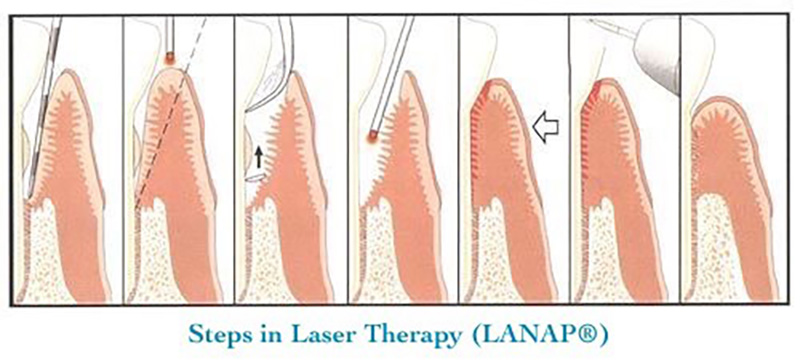
The Millennium Periolase (LANAP®)
We have the newest technology available for periodontic care: the Nd:YAG Millennium PerioLase. This is the latest generation of the Nd:YAG laser and it’s designed specifically to treat periodontal disease.

The new pulsed Nd:YAG laser can be used to safely remove the sulcular lining of periodontal pockets without damaging the subjacent connective tissue at the light of microscopic level. Laser periodontal therapy specifically targets the highly pathogenic black pigmented bacteria and is able to vaporize these bacteria safely because of a very rapid 1/10,000th of a second pulse that allows the tissue to cool 99.8% of the time. Tests have shown that 80 percent of sections showed 100 percent epithelium removal without damage to connective tissues. In a six-month follow-up study of laser treated subjects versus conventional surgery patients, researchers noted equal pulp vitality, gingival index, pocket depth reduction, and P. gingivalis and P. intermedia (periodontal pathogens) bacteria levels for both treated groups.
A newly developed procedure known as LANAP, (Laser Assisted New Attachment Procedure), is an FDA-approved procedure performed by the PerioLase. The objective of LANAP laser therapy is pocket reduction achieved by establishing a new connective tissue attachment to the tooth at a more coronal level. The LANAP procedure involves an environment in which new bone, cementum, and the PDL can form on a previously diseased root surface. LANAP allows us to treat periodontal disease in a minimally invasive procedure that eliminates the need, in most cases, for conventional blade surgery (osseous and flap surgery).
Clinical Advantages of the Periolase
- Efficiency & Precision
- Selective photo-thermal ablation
- Deeper Penetration/Aids in removing tarter
- Stimulates regeneration of tissue
- Neutralizes endotoxins/Bactericidal
- Hemostasis/Less sensitivity
- Quicker healing/Minimally invasive for optimum patient comfort
- Reduction in bleeding gums, bacteria, pain and bad breath
- Teeth and smile are maintained
- No stitches are needed
- Minimal pain
- Minimal downtime after treatment
- Minimal recession after treatment
In addition to the clinical benefits, the PerioLase laser treatment is also great for patients who have medical problems requiring drugs such as Plavix or Coumadin. Patients do not have to discontinue usage of these drugs with this laser therapy. These benefits make it ideal for patients who are fearful of conventional periodontal scaling and surgery. Of course, maintenance visits and good plaque control will be necessary following laser treatment.
Periodontal Pocket Sterilization
LASER therapy is incorporated as a modality of gum treatment against disease, or “periodontitis”. If periodontal disease is recognized in its early stages, laser gum treatment can be used and is extremely successful for gingival pocket sterilization. This simply means that the laser’s affinity for diseased tissue allows for vaporization of the diseased tissue and associated bacteria. The healthy tissue remains and can grow back to the tooth to provide for a manageable pocket depth with excellent dental hygiene. Laser gum treatment is performed under local anesthesia (novacaine) in conjunction with scaling and root planning (“deep cleaning”).
A newly developed procedure known as LANAP, (Laser Assisted New Attachment Procedure), is an FDA-approved procedure performed by the PerioLase. The objective of LANAP laser gum treatment is pocket reduction achieved by establishing a new connective tissue attachment to the tooth at a more coronal level. The LANAP procedure involves an environment in which new bone, cementum, and the PDL can form on a previously diseased root surface. LANAP allows us to treat periodontal disease in a minimally invasive procedure that eliminates the need, in most cases, for conventional blade surgery (osseous and flap surgery).
Patients come to our office to save their teeth from periodontal disease. While the goal of every periodontist is hopefully to save your teeth, it is important that you know there are different philosophies on treating periodontal disease Older treatment therapies would remove bone and gum to stop periodontal disease, usually resulting in painful root exposure and loose teeth. While some practitioners still employ these strategies to just halt periodontal disease, our commitment to you is to use therapies aimed at regenerating the tissues you have lost.
Regeneration is the process by which we are able to grow back the tissues lost through periodontal disease, like lost-bone, gum, and periodontal ligament, thereby restoring the beauty and function of your teeth and gums. What is probably of the greatest interest to you is that these regenerative procedures many times employ nonsurgical methods to accomplish their goals. Deep cleanings (scaling and root planing) or laser periodontal therapy comprises the majority of your treatment in our office. The way you benefit from this is that you get more conservative, more comfortable, more successful and less expensive treatment to save your smile. Regenerative measures can be taken in a number of ways, and which method is employed depends on the severity and presentation of your disease. Our goals when you finish treatment is to get you back to eating the foods you always enjoyed in the past, giving you back a smile that exhibits great confidence and having a mouth that is pain and disease free.
Gingivectomy
A gingivectomy is necessary when the gums have pulled away from the teeth, creating deep pockets. The pockets make it hard to clean away plaque. Gingivectomy is usually done before gum disease has damaged the bone supporting your teeth. The procedure involves removing and reshaping loose, diseased gum tissue to get rid of pockets between the teeth and gums. After removing the gum tissue, a putty-like substance is placed over your gum line. This will protect your gums while they heal. If you maintain good dental care after surgery, a gingivectomy is likely to stop gum disease.
Frenulectomy
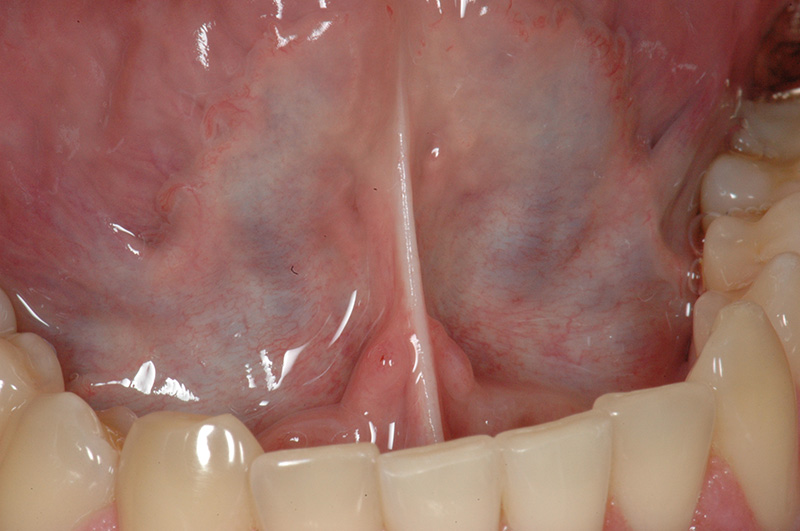
A frenulum is the fold of tissue that is visible when you pull your lip out away from your teeth or is seen attached to your tongue when you lift your tongue to the roof of your mouth. A frenulum serves no true physiological purpose; however, when it attached too close to your teeth, or in the case of being “tongue tied”, it is attached too close to the tip of your tongue, this can lead to recession, bone loss, root cavities and speech impediments. LASER gum treatment to correct frenulums is very quick and precise, and usually involves no “stitches” or bleeding. As with most LASER therapies, results are instantaneous.


Tongue Tie
It is estimated that up to 10% of babies are born with a tongue tie. This condition is when the strip of skin (frenulum) that connects the baby's tongue to the bottom of the mouth is too short. A baby born with a tongue tie can have problems, especially with breast feeding, as they are not able to open their mouth wide enough to feed properly. They can also have problems with tongue movement, and speech difficulty can occur as the child grows.
The treatment for a tongue tie is relatively simple, and can be performed with a local anesthetic if the baby is very young. The tongue tie is corrected with a laser, is very precise, and takes only a few seconds. There should be very little blood loss, and the baby can nurse immediately afterward.
Treatment for tongue tie can also be performed for older children, as well as adults, and is usually done with a general anesthetic and stitches if needed.

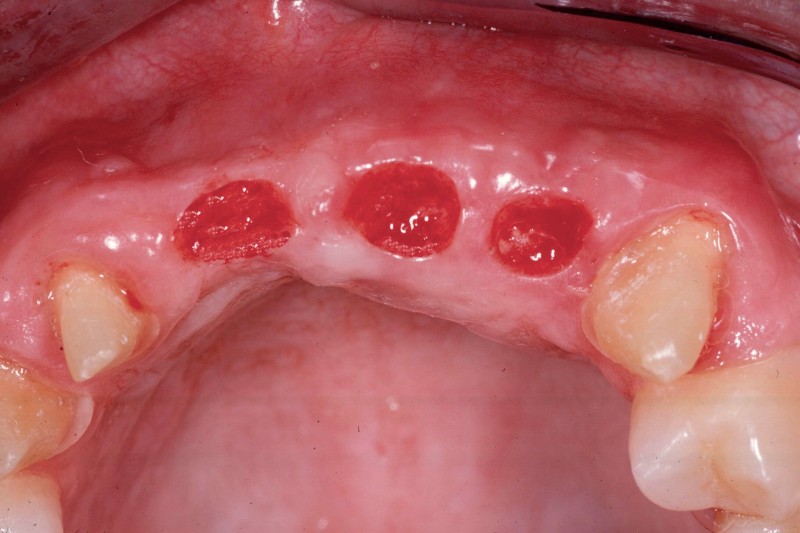
Pre-Prosthetic Procedures
Occasionally patients may require preparatory surgery to ready the mouth to accept a new dental prosthetic, whether be it a denture, bridge, or implants. Since a dental prosthesis (except dental implants) is placed over the edentulous ridge, the shape and dimensions of the ridge effects the form and function as well as esthetics of the final outcome. Pre-prosthetic surgery can be used to attain the desired foundation.
Such procedures may include:
- Bone Smoothing and reshaping
- Augmenting uneven ridges with bone or tissue grafting
- Extending the vestibule for better fit of dentures
- Removal of excess bone or tissue





Maintenance
Successful periodontal therapy with regular periodic maintenance care can sustain periodontal health and reduce tooth loss. Regular post-treatment maintenance regimen is successful in halting tooth loss in nearly 85 percent of patients. This regimen involves regular check-ups and detailed cleanings every three months to prevent repopulation of periodontitis-causing micro-organisms, and to closely monitor affected teeth so that early treatment can be given if disease recurs.
Our highly trained hygienists help patients create effective oral hygiene regimes that encompass the correct choice of toothbrush for them, brushing technique, flossing and use of a medicated mouthwash. Advice is also given on lifestyle factors such as smoking and diet that affect gum health.
Following active therapy, an interval is established for periodic ongoing care.
Maintenance procedures are performed under ongoing supervision and include:
- Update of medical/dental histories
- Extraoral & intraoral soft tissue exam
- Dental exam, cancer screening
- Periodontal exam
- Removing bacteria (plaque & calculus)
The successful long-term control of periodontal disease depends on active maintenance care through supportive periodontal treatment. A customized program will be "set-up" for you that will allow us to monitor for recurring disease and your plaque control efficiency.
Clean between your teeth
Dental floss or inter-dental brushes remove plaque and particles of food from between the teeth and under the gum line. These are areas that a toothbrush cannot reach. Correct technique is important, so ask for advice from your dentist or hygienist.
Use mouthwash
Fluoride mouthwashes can help to remineralize the enamel. Some antiseptic mouthwashes reduce the number of plaque bacteria. Those containing chlorhexidine is very effective, but can stain the teeth and affect the sense of taste in the long-term. Always follow your dentist's advice and read the instructions on the box or bottle.
Try disclosing tablets
These are small pills that, if crunched for 30 seconds, turn plaque a bright color - usually pink. This can help you to see any areas that you have missed.
Chew gum
Chewing sugar-free gum after a meal stimulates the production of saliva, which helps to neutralize plaque acid. Some chewing gums contain a sugar-free sweetener called xylitol, which suppresses certain types of plaque bacteria. Research is currently looking at whether this prevents decay.
Control sugar in your diet
There is a clear link between sugary food and drinks and tooth decay. Some types of sugar are worse than others. The biggest offenders are those added to food during manufacturing (refined sugars).
It is how often these sugars are eaten - rather than the amount - that is important. Avoiding refined sugars between meals gives your teeth a chance to be remineralized by saliva.
Fruit, vegetables, cheese, and milk all contain natural sugars that are much less likely to cause decay. This makes them a good alternative to sweets, and suitable for snacks between meals.
Alcohol and tobacco
Smoking stains the teeth and increases the risk of gum disease and tooth loss.4 Alcoholic drinks, and the mixers used with them, often contain lots of sugar, increasing the risk of tooth decay.
Drinking alcohol and smoking or chewing tobacco is also associated with an increased risk of developing mouth cancer.
