It is common for people to view their physical ailments and diseases as separate issues and not as something that is interconnected. I think it's possible to compare the human body to the world wide web. It is a system in which each part is integral to the other part; and when one part fails, the whole system is affected. The location of the malfunctions and the conditions that are causing the problem to worsen are important to identify. Also, in line with this idea is the relationship between periodontal disease and other systemic health issues in humans.
It is common knowledge that periodontal disease, also known as periodontitis or severe gum disease, is an infection and inflammation in the mouth, specifically the gums, which when left untreated can lead to tooth loss and bone loss. Despite its incurable nature, periodontitis can be managed through proper dental care. If not managed, the condition will worsen until total tooth loss occurs.
Aside from tooth loss, studies have shown that deep gum disease is associated with other health issues such as cardiovascular disease, diabetes, preterm birth, and arthritis. There has been extensive research linking systemic health issues and gum disease, even though it does not appear to be a cause-and-effect relationship.
Most systemic health issues associated with periodontal disease have an inflammatory component. In the mouth of a human, billions of bacteria are present every day. There are some types of bacteria that are helpful and work to keep the teeth and gums healthy, while others are harmful and work to destroy the teeth themselves, the roots, including the bones. The harmful bacteria left in the mouth will eventually develop into something worse, such as periodontitis. When the infection sits in the mouth and gums, it begins to cause severe inflammation. Additionally, this inflammation may exacerbate other critical health issues in addition to being painful and damaging to your teeth and jaw bone.
"Despite its incurable nature, periodontitis can be managed through proper dental care. If not mangaed, the condition will worsen until total tooth loss occurs."
DR. KAMRAN HAGHIGHAT, B.D.S., M.S., P.C.
Diplomate, American Board of Periodontology
Diplomate, American Board of Oral Implantology
Cardiovascular Disease and Periodontitis
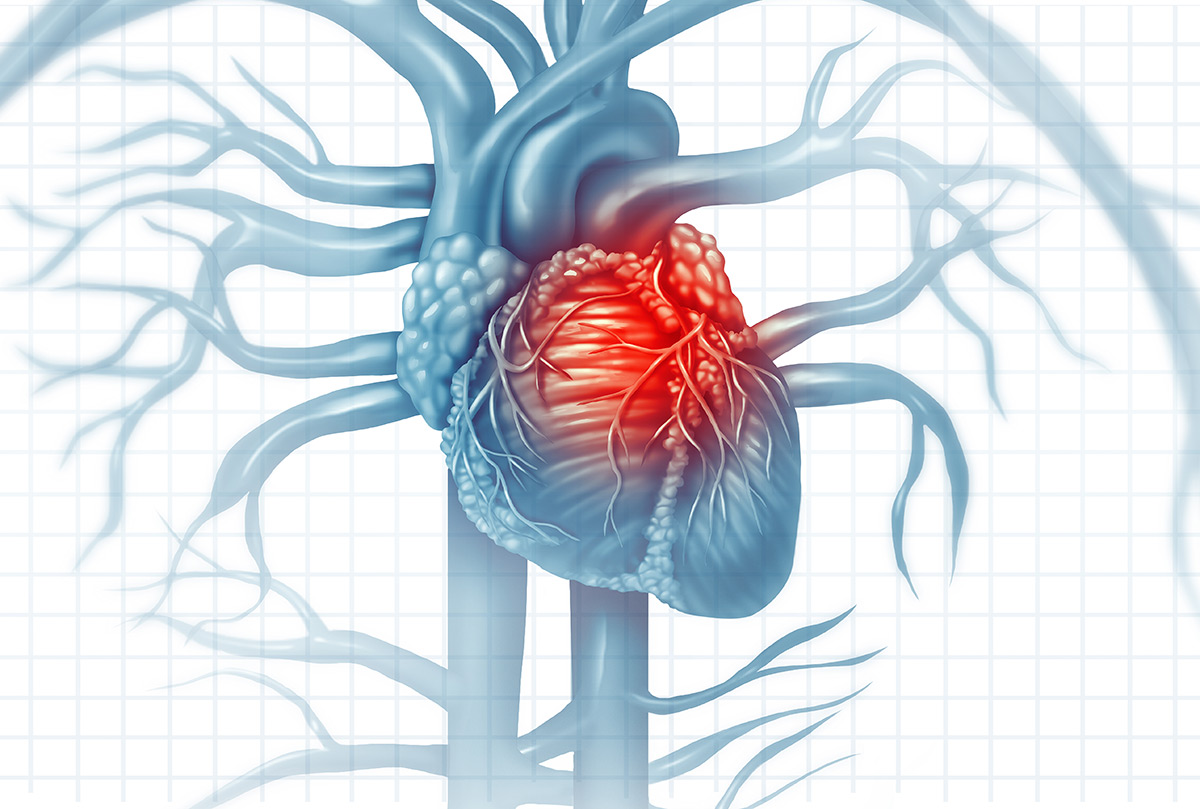
It is estimated that there is a 19% increase in cardiac disease risk associated with periodontal disease among individuals over the age of 65. This figure reaches 44% among those over 65. In spite of how challenging it is for people to imagine that their dental health can negatively affect their overall health, the connection between your body, the nerves, and the bloodstream cannot be ignored.
It is possible for infections from the mouth to travel through the bloodstream to the heart and cause inflammation of the valves that surround the heart. In a recent study, Periodontal Diseases and Cardiovascular Events: Meta-Analysis of Observational Studies, it was found that subjects with periodontal disease had a significantly higher risk of cardiovascular disease (34%). A variety of factors can contribute to heart disease, but periodontitisPeriodontal Disease increases a person's risk. Treatment of periodontitis does not, however, reverse cardiovascular disease. There is still a need for research in that area.
Diabetes Mellitus and Periodontitis
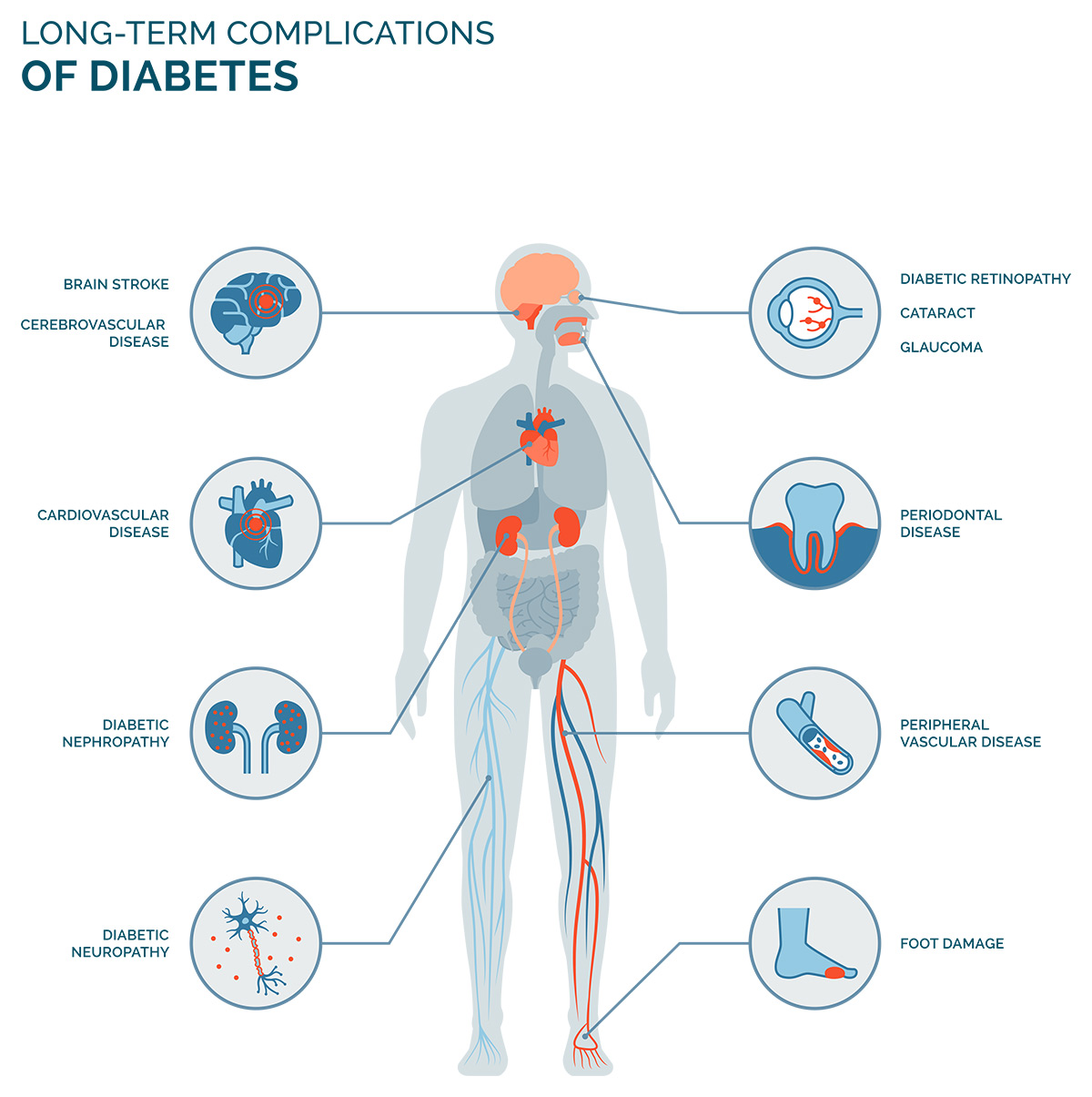
A study by Muhammad Ashraf Nazir found that people with type 2 diabetes and severe periodontitis had 3.2 times greater mortality risks than people without periodontitis or with mild periodontitis.
Severe gum disease is characterized by a high level of inflammation. Chronic pain and swelling of the gums follow. Other parts of the body will be affected by the inflammation, particularly those afflicted with other diseases such as diabetes mellitus.
Several studies have been published in the National Library of Medicine that provides evidence suggesting a connection between severe gum disease and diabetes mellitus. Gustavo G. Nascimento and associates reviewed 13 of these studies. A total of 49,266 individuals participated in the study, with 3,197 diagnosed with diabetes. They concluded that diabetes significantly increased the risk of developing periodontitis or advancing it by 86%. Although this is significant, there is no evidence that they are mutually exclusive.
Inflammation caused by diabetes can lead to periodontal flare-ups and worsen the oral disease. A person's gum disease will likely improve when their diabetes is properly controlled. Nevertheless, caring for diabetes does not guarantee the eradication of periodontitis.
Other Systemic Issues and Periodontal Disease
Rheumatoid Arthritis and Periodontal Disease
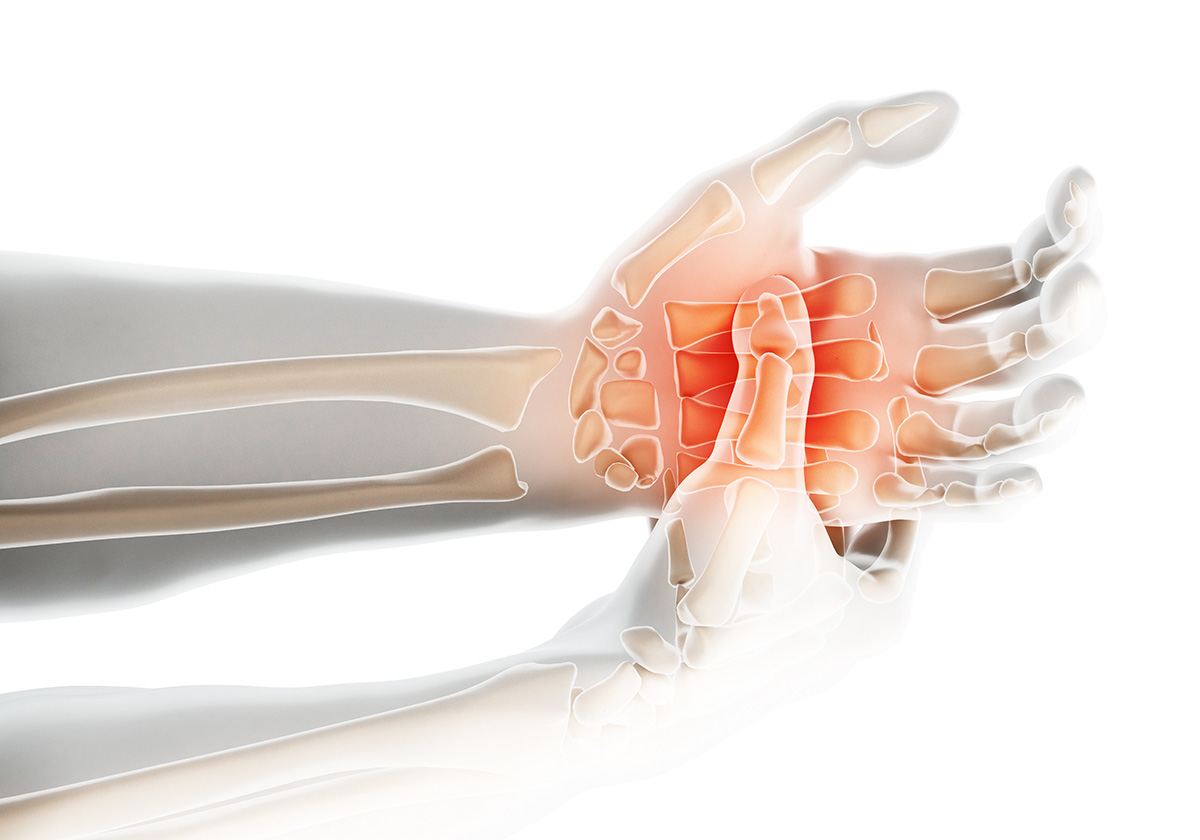
Researchers have found that rheumatoid arthritis is associated with periodontal health when tooth loss of the alveolar bone occurs. Approximately 20 bacterial species that live in the subgingival have been associated with periodontal disease among the millions of bacteria inhabiting the mouth. Leaving this bacteria untreated will result in tooth loss.
Rheumatoid Arthritis is a chronic inflammation that affects the joints and causes difficulty in movement. Evidence has shown that inflammatory flare-ups with Rheumatoid Arthritis and periodontal disease go hand-in-hand with causing the issue to worsen, since both trigger inflammation.
In a study published by Jacqueline Detert and colleagues, "patients with longstanding active Rheumatoid Arthritis have a significantly higher incidence of periodontal disease when compared to healthy individuals and that people with periodontal disease have a higher prevalence of Rheumatoid Arthritis than people without periodontal disease." Alveolar bone loss and tooth loss are common symptoms in people with these diseases, indicating that these diseases are closely linked.
Birth Risks and Periodontal Disease
Premature births, low birth weights, and even pre-eclampsia have been closely related to periodontal disease. As a result of periodontitis, oral bacteria produce a labor-inducing compound known as prostaglandin. During pregnancy, a pregnant woman's prostaglandin levels may rise due to periodontitis, which may lead to premature delivery. The presence of an elevated level of prostaglandin can result in premature births and low birth weights.
In addition to birth risks and periodontitis, elevated levels of C-Reactive Protein (CRP) are often associated with these conditions. Periodontal infections will raise CRP levels, which will lead to heightened inflammation in the body. As a result, inflammation in the arteries can cause strokes or heart attacks, as well as premature birth or pre-eclampsia in pregnant women.
In the journal, Evidence-Based Dentistry, Jean-Noel Vergnes reported that “six studies, representing a total of 3,420 women (493 pre-eclamptic and 2,927 non-pre-eclamptic control women) were pooled for meta-analysis. Women with evidence of periodontal disease during pregnancy had a 1.76 fold higher risk of pre-eclampsia compared with women without periodontal disease.”
The hormonal imbalances and changes associated with pregnancy can make periodontitis a problem for expectant mothers. If left untreated, these hormones can lead to gingivitis, which will turn into periodontal disease, causing a host of problems during pregnancy. It is imperative to rule out periodontal disease during pregnancy and to treat or maintain it as soon as possible if it is found.
A serious oral health concern, periodontitis can affect more than just teeth. The importance of proper dental care routines and regular dental visits cannot be overstated. To catch periodontal diseases before they become severe, you should see a periodontist if any significant symptoms appear.






